Healthbeauty123.com – A child suffering from Chiari malformation is at risk for undergoing brain decompression surgery. This condition causes the brain stem and cerebellum to become pushed downward into the upper spinal canal, which in turn can affect the functions controlled by these parts of the brain. The problem can also block the flow of cerebrospinal fluid, which surrounds and cushions the spinal cord. A neurosurgeon has been monitoring Abby’s condition closely for several years, and he suggested brain decompression surgery.
Increasingly Popular Treatment Options
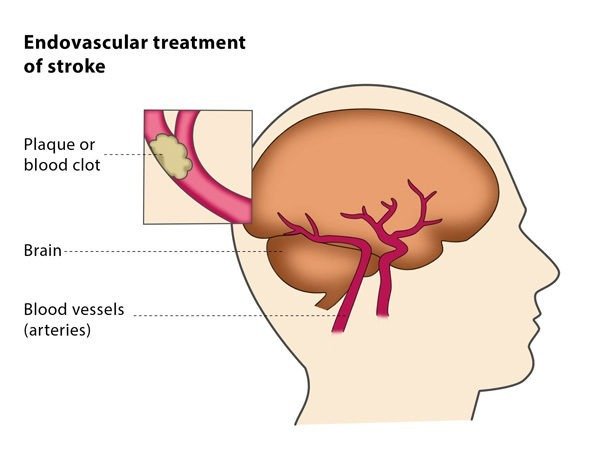
In a recent study, researchers compared time taken from ED admission to brain decompression. Bypassing CT at a local hospital and completing the procedure at a larger center, the study significantly shortened the time to care. Decompression time was reduced by a median of 51 minutes. Overall, this study showed that pre-alerting neurosurgeons and using advanced technologies such as ultrasound during the CT procedure were key factors in improving patient outcomes.
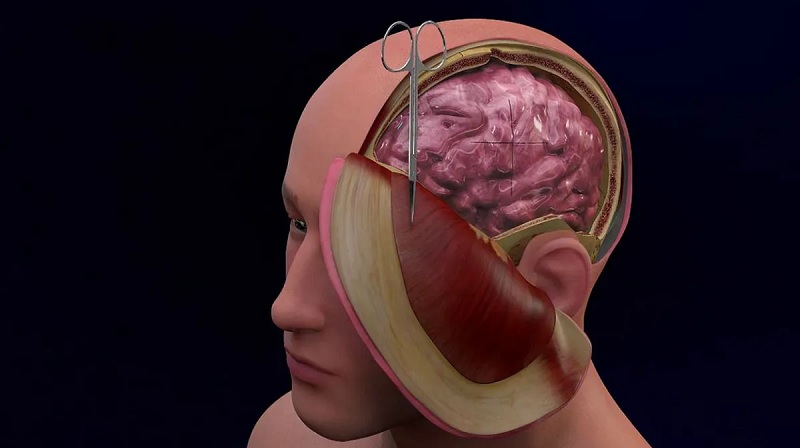
While craniotomies are generally the last resort in neurosurgery, decompression with dural augmentation is an increasingly popular therapeutic option. Among the many potential complication of DC, the major one is intraoperative brain extrusion. However, a new surgical technique, termed “gradual and controlled decompression,” is developing to address this issue. The new technique is also being tested to treat patients with chronic conditions, including stroke.
The first large DC was reported in the United States in 1896 by Kocher, a neurologist who studied the effects of traumatic brain injury on CSF circulation and cerebral blood flow. He advocated trephination in all cases of intracranial hypertension and suggested temporary hemicraniectomy in selected cases. A similar method was proposed by US neurosurgeon Cushing for the treatment of other brain disorders, including stroke and traumatic brain injury.
Procedure to Reduce Stroke Risk
Patients who had undergone DC underwent cranioplasty between two weeks and eight months afterward. In these cases, an autologous bone flap was used. This procedure is performed if the patient’s swelling has been significantly reduced. If the procedure had reduced the risk of stroke, the patient may be able to undergo cranioplasty before discharge. This procedure, however, may be performed only if the patient’s general health and anesthesia have been evaluated favorably.
While there are no definitive treatment regimens for pediatric patients with severe head injuries, the presented study adds to the argument for the use of surgical decompression in the early stages. This study calls for a controlled trial of this procedure in pediatric severe head injury patients. The study findings also demonstrate that DC is an effective method to manage cerebral edema. If you’re wondering how much the risk of brain damage is, read on!
In the past, DC has been associated with poor clinical outcomes. There are only 22 publications from 1960 to 1980 that specifically studied the use of DC for TBI patients. Mortality rates ranged from 46% to 96%. The main surgical techniques involved the removal of the periosteum and removing the temporal muscle. There are two main types of DC. They vary in length and location. The most common form of DC in pediatric patients involves a right-sided craniotomy.
Surgical Decompression Can Be Done In Several Ways
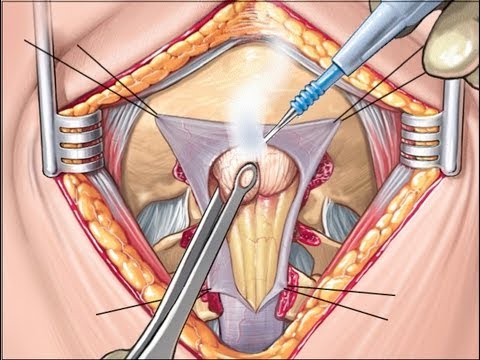
There are various methods of brain decompression. One method used is cerebral angioplasty. Surgical decompression can be performed in a number of ways. For example, one method may use an adhesive sheet to reduce blood clots. Another method is to apply a silicone elastomer sheet. In both cases, the procedure can reduce postoperative bleeding and infection. Although surgical decompression is a surgical procedure, it may have a limited impact on brain edema.
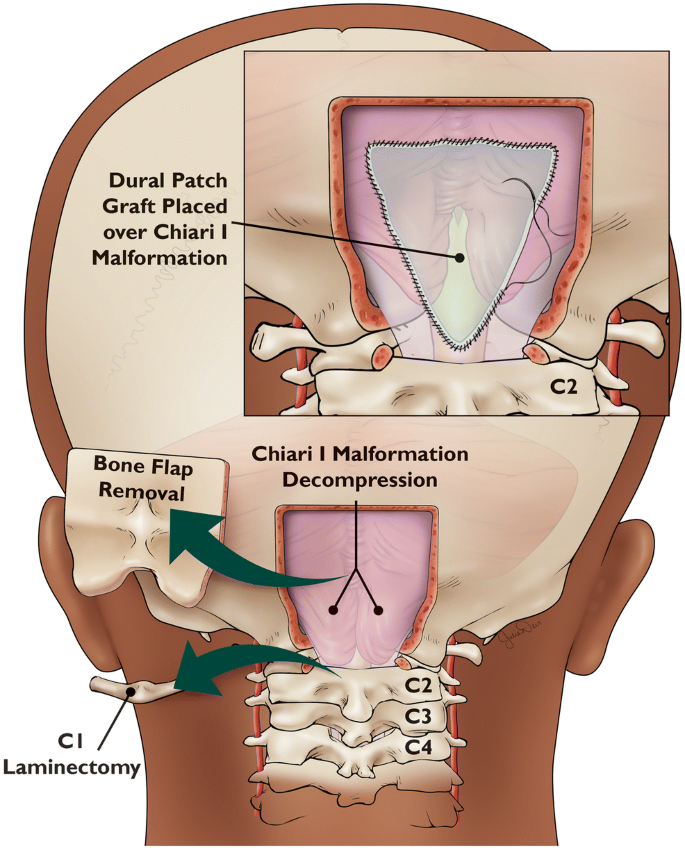
In severe cases, an additional piece of the temporal bone may be removed from the temporal floor or squamous part of the brain. An incision is made in the dura, one cm away from the edge of the bone. The exposed brain cortex is covered with a silicone sheet called DuraGen. After removing the myocutaneous flap, a silicone elastomer sheet is inserted between the dura and the myocutaneous flap. After a few days, the bone will be sufficiently covered by the silicone sheet.
Reference: